Mitral Valve Prolapse or MVP is a heart condition in which the heart’s mitral valve fails to close properly, it will cause the blood to flow backward into the left atrium when the heart pumps the blood. Although it is benign in most cases, Mitral Valve Prolapse may pose unique challenges to professional athletes, especially on sports that involves extensive physical activity.
The physical demands during competitive sports can trigger or worsen Mitral Valve Prolapse symptoms. Making it a important for athletes, coaches, and trainers to understand the implications for athletes to ensure both the safety and performance of athletes.
MVP is often caused by genetics, that leads to unusual valve leaflet structure. Other common causes of MVP includes aging, rheumatic heart disease, and heart attack.
Symptoms of MVP are often minor, with most people who have MVP are asymptomatic. However, some people may experience palpitations, shortness of breath, fatigue, and even chest pain. Diagnosis of Mitral Valve Prolapse is usually done through echocardiography, which can help identify the abnormal mitral valve movement.
The Impact of MVP on Athletes Performance
High intensity sports requires robust cardiovascular function. The increased of oxygen demand during physical exercise requires the heart to work even harder, making it imperative for all cardiac structures to function optimally.
In athletes, MVP might lead to decreased cardiac output, which can compromise performance. Additionally, arrhythmias associated with MVP may increase the risk of sudden cardiac events during intense physical exercise.
Risk Factors in Athletes with MVP
Identifying potential risks associated with MVP in athletes can guide risk mitigation strategies.
1. Sudden Cardiac Death (SCD) and its Association with MVP
While rare, SCD is a serious risk associated with MVP, particularly in the context of competitive sports. Intense physical activity might increase the risk of ventricular arrhythmias in athletes with MVP, leading to potential cardiac events.
2. MVP, Arrhythmia, and Endurance Sports
Endurance sports, characterized by prolonged periods of physical exercise, may particularly increase MVP-associated arrhythmias, necessitating careful management of athletes with MVP who participate in these sports.
Recommendations for Sports Participation

After recognizing the risks, the focus shifts towards formulating strategies for safe sports participation.
1. Regular Monitoring and Check-ups
Regular cardiac evaluations, including echocardiography, can help monitor the progression of MVP in athletes, enabling timely intervention. Athletes should undergo these assessments annually, or more frequently if symptoms worsen.
2. Sport-Specific Recommendations
Certain sports may pose less risk than others for athletes with MVP. Generally, low-intensity and non-contact sports are safer. However, participation should be individualized, considering the severity of MVP and the athlete’s overall health.
3. Impact of Medical Treatment on Athletic Performance
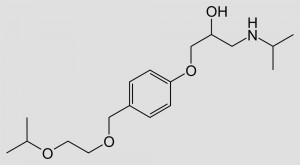
Treatment for MVP, such as beta-blockers or valve repair surgery, can impact an athlete’s performance. Healthcare providers should consider these impacts while devising a treatment strategy, aiming to minimize performance interference.
Adapting Training Regimens for MVP Athletes
Altering training routines to suit an athlete’s physical condition is an important aspect of MVP management.
1. Cardiovascular Exercise Modifications
Athletes with MVP should tailor their cardiovascular exercise to their individual tolerance, focusing on maintaining heart rate within safe limits and avoiding excessive strain.
2. Strength Training Modifications
Strength training can be beneficial, but athletes with MVP should avoid extreme isometric exercises, which can increase cardiac load.
Lifestyle Changes for Athletes with MVP
Implementing lifestyle changes can complement medical interventions in managing MVP. A balanced diet, stress management can help in mitigating MVP symptoms.
1. Dietary Considerations
A heart-healthy diet, rich in whole grains, lean protein, fruits, and vegetables, can help manage MVP symptoms. Athletes should also ensure adequate hydration and avoid excessive caffeine and alcohol.
2. Stress Management and its Importance
Stress can worsen MVP symptoms. Athletes should adopt effective stress management strategies, including mindfulness techniques, adequate rest, and balanced work-play schedules.
The Role of Coaches and Trainers
Coaches and trainers are crucial in supporting athletes with MVP. Their role includes recognizing symptoms, providing necessary guidance, and offering emotional support.
Coaches and trainers should be aware of MVP symptoms and be prepared to respond appropriately to signs of cardiac distress in their athletes.
Coaches and trainers play a key role in providing emotional and psychological support to athletes with MVP, fostering a positive environment and helping athletes manage their condition effectively.
Case Studies
Learning from successful athletes with MVP can inspire and guide others who are struggling with the same condition.
Despite the challenges, many athletes with MVP have achieved significant sporting success. These examples serve as motivation and reassurance for others dealing with the same condition.
An analysis of successful athletes with MVP can provide valuable insights into effective strategies for balancing competitive sports participation with MVP management, underscoring the potential to excel despite their heart condition.
Conclusion
Despite the challenges it presents, MVP doesn’t necessarily spell the end of a sporting career. With informed guidance, regular monitoring, and sensible modifications, athletes with MVP can continue to participate in competitive sports.
Regular check-ups, sport-specific recommendations, tailored training regimens, lifestyle modifications, and effective support systems are crucial elements of safe and successful sports participation for athletes with MVP. By following these strategies, we can ensure that our athletes continue to perform to their utmost potential, while managing their health optimally.



Leave a Reply